New findings: Lack of certain friendly gut bacteria may worsen COVID
COVID-19 has made the human immune system a household conversation. And many have done their own research and found that natural immunity and, indeed, health have a strong link to the gut.
 It’s now more important than ever to be aware that scientists are observing significant alterations in the gut microbiome in those with COVID-19 and/or in those recovering.1
It’s now more important than ever to be aware that scientists are observing significant alterations in the gut microbiome in those with COVID-19 and/or in those recovering.1
Scientific researchers have uncovered a connection between particular strains of gut bacteria and the severity of COVID-19.2
Introducing strategies to bolster immune system health and maintain a balanced gut microbiome should be a high priority.
Or to be even more precise, strategies that alter the intestinal microbiota could reduce disease severity.
A significant study has revealed key findings on severe COVID in an individual and how the infection impacts their microbiome.
Disturbances in certain gut bacteria can make COVID worse
Scientists are discovering that there’s a reduction of an important anti-inflammatory species — Faecalibacterium prausnitzii — in patients with COVID-19.1 Reduced Faecalibacterium prausnitzii means lowered butyrate production and more inflammation since. F. prausnitzii helps control inflammation.
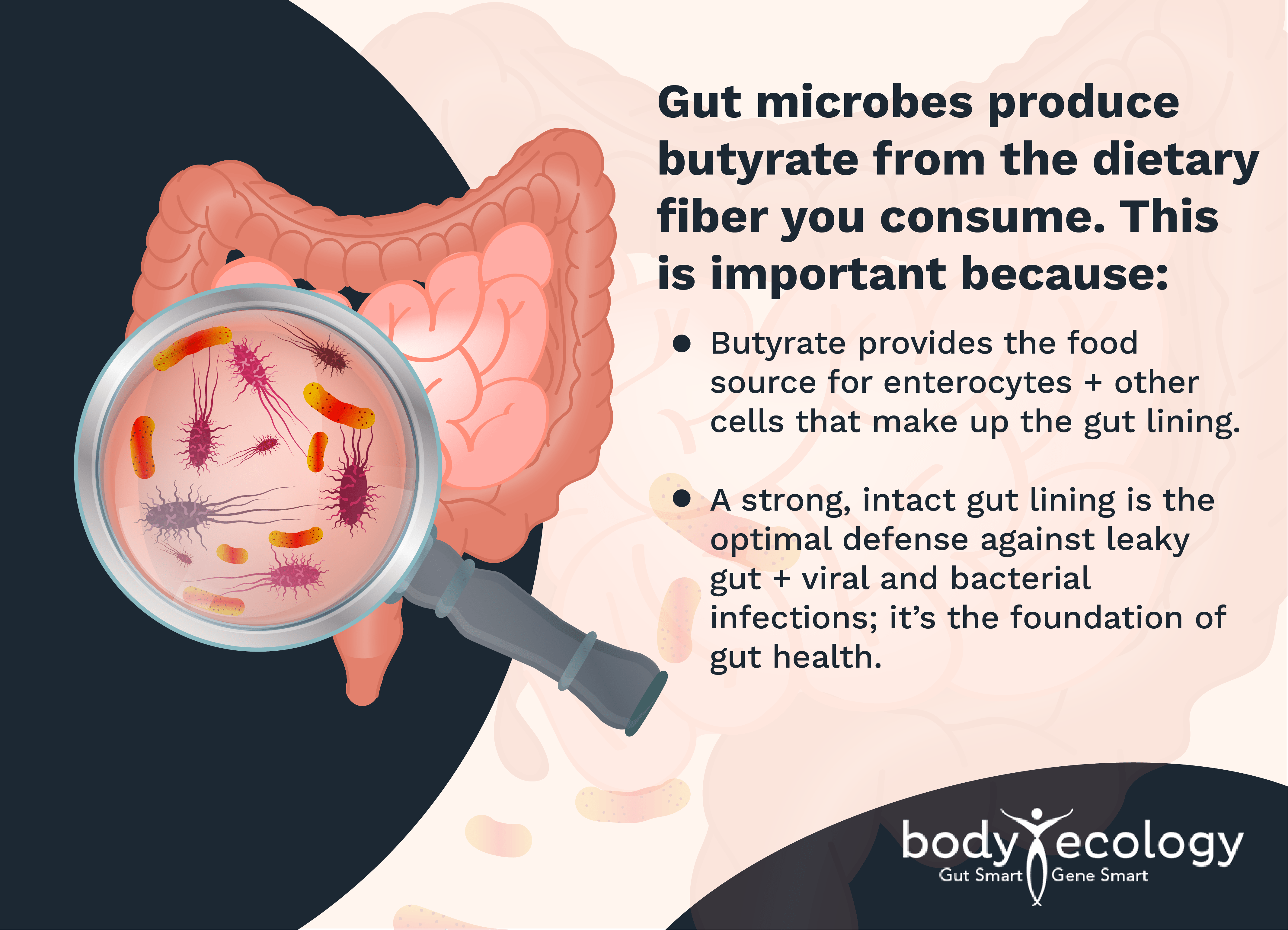
Furthermore, loss of Faecalibacterium prausnitzii lowers levels of Bifidobacteria since these two bacteria are great pals. Low levels of Faecalibacterium prausnitzii and Bifidobacteria have been shown to linger for weeks after a patient’s hospitalization — and that can mean an increase in the severity of systemic inflammation, which underlies all diseases.
If you’re a COVID long hauler, this is important to know.
We’ve got a freebie with your name on it. Here’s where you can download our gut health guides for free.
A pilot study out of China conducted in September of 2020 analyzed stool samples in 15 patients in Hong Kong from February 5 through March 17, 2020.1 Samples were taken two to three times per week from the time patients were admitted to the hospital until discharge.
In the study:
- The severity of COVID-19 in these 15 patients was categorized as mild (X-rays revealing no pneumonia), moderate (with pneumonia present), and severe (with a respiratory rate of greater than 30 breaths per minute and/or oxygen saturation less than 93 percent when breathing on their own), or critical (respiratory failure with the patient ventilated, in shock, or with organ failure requiring intensive care).
- Microbiome data collected from these COVID-19 patients were compared with microbiome data from six subjects with non-COVID-related pneumonia, as well as 15 healthy individuals who served as the control group. The gut microbiome data in the groups were analyzed then compared with the severity of the disease. Changes in the shedding of the virus in the patient’s stool were analyzed.
- Data analyzed from the microbiome of the 19 COVID-19 patients (by looking at their stool samples) showed significant changes in their microbiome compared with controls. These samples also revealed higher than normal levels of pathogenic organisms and lower than normal levels of beneficial bacteria at the time they were hospitalized and throughout their stay in the hospital.
Depleted beneficial bacteria and gut dysbiosis continued in these patients once they had recovered from the SARS-CoV-2 infection.
High levels of certain species, such as Coprobacillus, Clostridium ramosum, and Clostridium hathewayi bacteria, were connected with the severity of COVID-19. Low levels of Faecalibacterium prausnitzii were associated with the more severe COVID cases. (Remember, F. prausnitzii is an anti-inflammatory bacterium.)
During hospitalization, patient stool samples were analyzed and found to contain another common species of gut microbes called Bacteroides (Bacteroides dorei, Bacteroides thetaiotaomicron, Bacteroides massiliensis, and Bacteroides ovatus).
Bacteroides species are opportunists — can be significant clinical pathogens — and are typically in most anaerobic infections when the environment of the gut has infection and inflammation.
However, in this study:
- Scientists found that changes in the gut microbiome elicited changes in ACE2 receptor function, allowing for the infection to enter the body more easily and with increasing severity.
- Researchers concluded that strategies that positively alter the terrain of the GI tract, impacting the intestinal microbiota in a good way, might reduce the severity of the disease.
Of course, our first suggestion would be to alter the terrain by eating the right fermented foods and drinks. And since Faecalibacterium prausnitzii and Bifidobacteria are good friends, it simply makes sense to replenish Bifidobacterium in the gut.
Body Ecology offers two potent formulas that help restore lost Bifidobacteria while recovering from mild to severe COVID:
- Body Ecology’s GI Distress Relief Probiotic provides a proprietary blend of two well-researched strains of Bifidobacterium and a prebiotic food source to nourish them. Added to these two Bifido is Saccharomyces boulardii, a beneficial yeast that research shows helps reduce gliotoxin, a dangerous toxin produced by candida and mold that suppresses the immune system.3
- Body Ecology’s Bifidus Power Blend is another high-dose combination of four bifidobacterial strains and comes in powder form, making it easy to dose at higher levels when needed. It’s also easy to give to children and even babies. It contains 75 billion microbiota per serving. Refrigerate this probiotic to maintain its level of potency.
More studies focusing on the impact of COVID-19 on gut health are currently in review and should publish soon.
Do this to increase Faecalibacterium prausnitzii
F. prausnitzii is not available as a probiotic supplement, but when many Bifidus are in the environment, F. prausnitzii will be there too.4 Most likely, manufacturers will never encapsulate F. prausnitzii because they’re so oxygen-sensitive that they die with air exposure.
Of course, like the other gut microbes, this little hero does need to be fed. If not, he dies out, and studies have shown that lower levels are associated with chronic constipation, celiac disease, IBS (Crohn’s and colitis), colon cancer, psoriasis, and type 2 diabetes.5-7
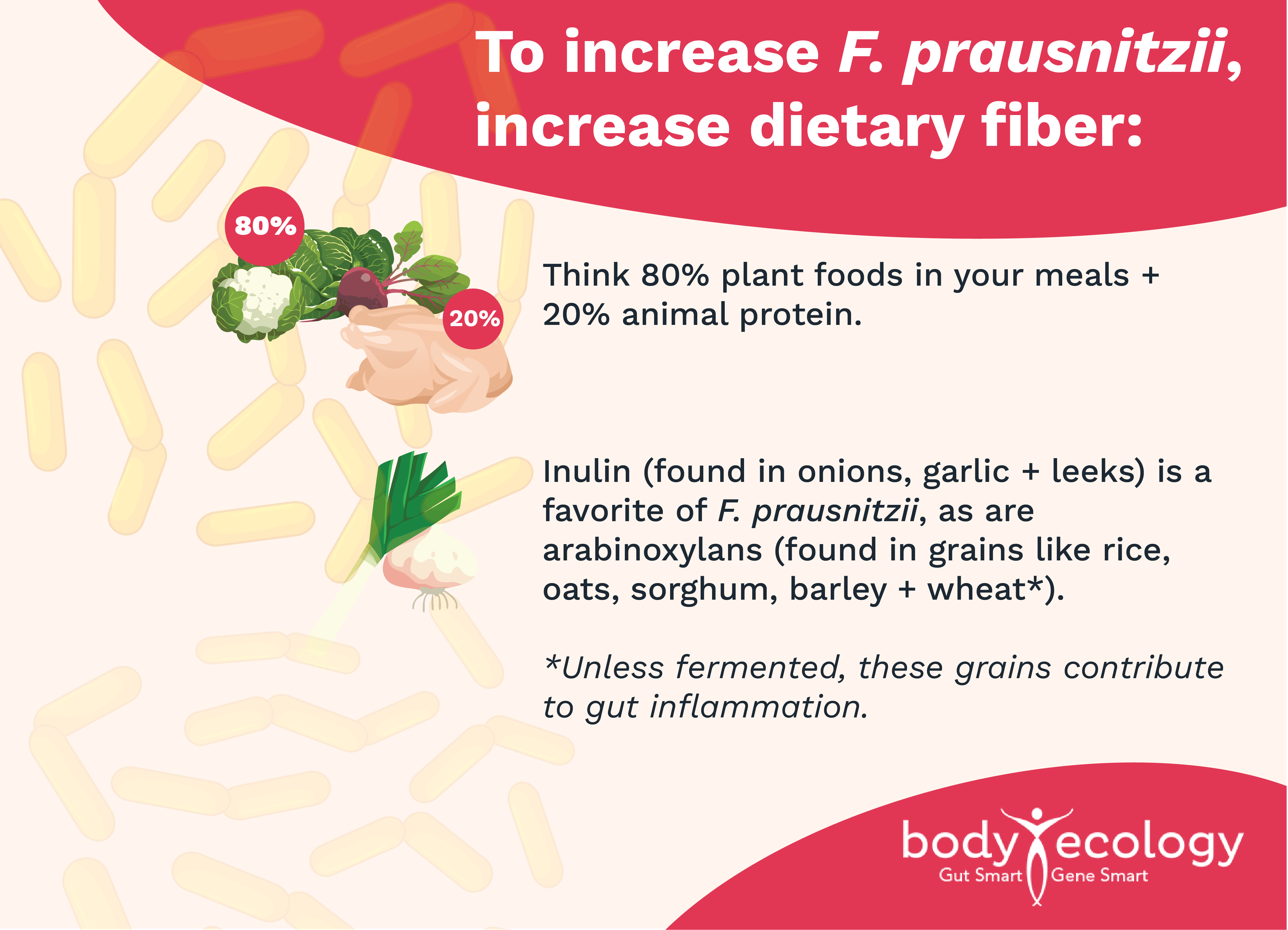
Body Ecology has always recommended a plant-rich diet (yet mindful of high-oxalate foods).
Bifidobacteria and F. prausnitzii like to hang out together and cross-feed each other. Since both increase with inulin, you can simply add Body Ecology’s EcoBloom™ to drinks, salad dressings, soups, your morning coffee, or just sprinkle it on anything to increase the number of Bifidus and F. prausnitzii.
REFERENCES:
- 1. Zuo T, Zhang F, Lui GCY, Yeoh YK, Li AYL, Zhan H, Wan Y, Chung ACK, Cheung CP, Chen N, Lai CKC, Chen Z, Tso EYK, Fung KSC, Chan V, Ling L, Joynt G, Hui DSC, Chan FKL, Chan PKS, Ng SC. Alterations in Gut Microbiota of Patients With COVID-19 During Time of Hospitalization. Gastroenterology. 2020 Sep;159(3):944-955.e8. doi: 10.1053/j.gastro.2020.05.048. Epub 2020 May 20. PMID: 32442562; PMCID: PMC7237927.
- 2. Yeoh YK, Zuo T, Lui GC, et alGut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19Gut 2021;70:698-706.
- 3. Miller LE, Lehtoranta L, Lehtinen MJ. The Effect of Bifidobacterium animalis ssp. lactis HN019 on Cellular Immune Function in Healthy Elderly Subjects: Systematic Review and Meta-Analysis. Nutrients. 2017 Feb 24;9(3):191. doi: 10.3390/nu9030191. PMID: 28245559; PMCID: PMC5372854.
- 4. Rivière, A., Selak, M., Lantin, D., Leroy, F., & De Vuyst, L. (2016). Bifidobacteria and Butyrate-Producing Colon Bacteria: Importance and Strategies for Their Stimulation in the Human Gut. Frontiers in Microbiology, 7. doi:10.3389/fmicb.2016.00979.
- 5. Lopez-Siles, M., Duncan, S. H., Garcia-Gil, L. J., & Martinez-Medina, M. (2017). Faecalibacterium prausnitzii: from microbiology to diagnostics and prognostics. The ISME Journal, 11(4), 841–852. doi:10.1038/ismej.2016.176.
- 6. Lopez-Siles M, Martinez-Medina M, Surís-Valls R, Aldeguer X, Sabat-Mir M, Duncan SH, Flint HJ, Garcia-Gil LJ. Changes in the Abundance of Faecalibacterium prausnitzii Phylogroups I and II in the Intestinal Mucosa of Inflammatory Bowel Disease and Patients with Colorectal Cancer. Inflamm Bowel Dis. 2016 Jan;22(1):28-41. doi: 10.1097/MIB.0000000000000590. PMID: 26595550.
- 7. Eppinga H, Sperna Weiland CJ, Thio HB, van der Woude CJ, Nijsten TE, Peppelenbosch MP, Konstantinov SR. Similar Depletion of Protective Faecalibacterium prausnitzii in Psoriasis and Inflammatory Bowel Disease, but not in Hidradenitis Suppurativa. J Crohns Colitis. 2016 Sep;10(9):1067-75. doi: 10.1093/ecco-jcc/jjw070. Epub 2016 Mar 12. PMID: 26971052.