READ THIS Before You Take Antibiotics For A Sinus Infection
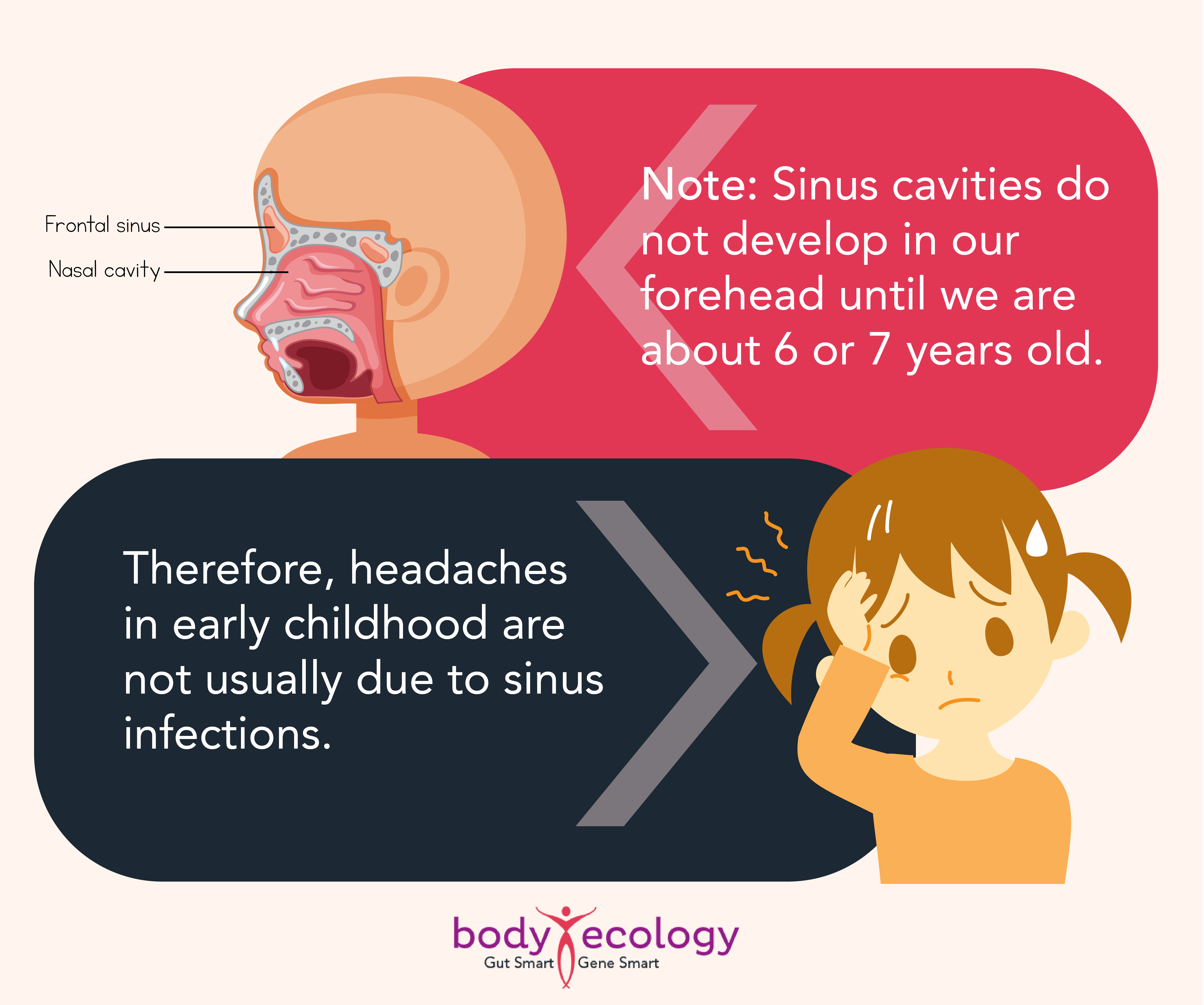
During cold and allergy season, many people suffer with sinus pain and pressure. Sinuses are four sets of hollow, moist air spaces in your cheekbones, your forehead, behind your nasal passages, and deep in your brain.
When the mucous membranes of your sinuses become infected or irritated, the infection is called sinusitis.
Causes & Common Treatments for Sinusitis
Sinus infections are traditionally thought to occur when a cold doesn’t clear up, or when you have severe allergies. Symptoms of sinusitis can include a daytime cough that’s “dry” and doesn’t improve after seven days, fever, dental and/or ear pain, tenderness in the face, nausea, headaches, and pain behind the eyes.
Common treatments for sinusitis include decongestants that reduce the swelling of the inflamed mucus membrane, pain relievers like aspirin and ibuprofen, and prescription antibiotics to kill bacteria.
Unfortunately, many people continue to experience sinusitis symptoms on a regular basis, even after taking antibiotics and over-the-counter medicines. This is because in many cases, the infection is not bacterial. In fact, over one in five antibiotics prescribed for sinusitis are frequently prescribed inappropriately, often for convenience.¹
For people who suffer from chronic sinusitis, the illness plus the strain on their body from too many antibiotics can leave them feeling pretty miserable.
Chronic Sinusitis: Is Fungal Infection to Blame?
While many doctors turn to antibiotics to heal chronic sinusitis, antibiotics may be ineffective. This is because studies show that fungal infections, not bacterial infections, may actually cause a large number (potentially, most cases) of chronic sinus infections.²⁻⁴
This became evident as early as 1999 when the Mayo Clinic published a study suggesting that fungal sinusitis was more common than previously thought. In the nasal washings from the sinuses of patients with chronic sinusitis, 96 percent of those studied had a fungal overgrowth in their sinus cavities.²
The disease is now known as EFRS (eosinophilic fungal rhinosinusitis) or EMRS (eosinophilic mucinous rhinosinusitis). Additionally, invasive fungal rhinosinusitis also has the potential to spread, moving from the sinus cavity.
Additional findings from the Mayo Clinic study:
- The control subjects who did not have sinusitis still had an overgrowth of fungus.
- However, the miserable patients suffering from sinusitis symptoms had a type of white blood cell called an “eosinophile” that was active.
- The eosinophils released a product called MBP (Major Basic Protein) into the mucus lining. This MBP attacks and kills the fungus but is also extremely irritating to the lining of the sinuses. MBP injures the lining of the sinuses and allows bacteria to proliferate.
Fungal infections do not respond to antibiotics at all, and antibiotics may actually make fungal infections worse.
Treat the Underlying Cause of Your Chronic Sinusitis
The injury to the lining of the sinuses by the fungus led to the now-popular belief that treatment of chronic sinusitis should be directed at the fungus, rather than the bacteria.
Since antibiotics don’t work and common treatments only temporarily alleviate symptoms, you need to address the underlying cause of your sinusitis, which may be the fungal infection with active white blood cells that produce the irritating MBP.
The misuse of antibiotics, a high-sugar diet, stress, birth control pills, cortisol, and other drugs (including recreational drugs and alcohol) all cause an overgrowth of fungi. Exposure to mold and fungi in the environment — both due to water leaks from roofs and plumbing, as well as more efficient homes with less air exchange — are also culprits.
The CDC now warns that antibiotic-resistant fungi are a major health threat.⁶
Consider these alternatives to conventional antibiotic treatment:
- Antifungal Diet – Antibiotics wipe out good and bad bacteria, so when you must use one, be sure you’re on an antifungal diet. And, take care to replenish the beneficial bacteria in your gut with fermented foods and beverages. CocoBiotic is a favorite daily probiotic power shot and mixer.
Shop prebiotic & probiotic supplements to help replenish the beneficial bacteria in your gut, helping to fight antibiotic resistance.
- Natural Remedies – There are options besides antibiotics that can be useful, especially if your immune system is strengthened from eating a probiotic diet. Colloidal silver, oil of oregano, and olive leaf extract are just three of many natural remedies worth researching for yourself.
- Facial Steams – Steam your face twice a day, and put antifungal essential oils in the water. (We love the selection from our friends at Vibrant Blue Oils.)The moist heat relieves symptoms and provides needed moisture for your nasal passages, made more soothing when using oils that are antifungal and antibacterial.

How an Antifungal Diet May Help Chronic Sinusitis
Diet is key when your sinus infection is fungal-based. A diet must be antifungal, like what you’ll find in the Body Ecology program.
Body Ecology is a system of health and healing that emphasizes the positive side of healing by introducing beneficial bacteria into your body versus killing bacteria with antibiotics.
While at times, we know antibiotics may be necessary for conquering a virulent bacterial infection, we believe in focusing first and foremost on prevention and on building a hardy immune system. We do this by establishing a healthy inner ecosystem (made up of friendly microbes) in your intestines. These help keep you strong so you have a much better chance of resisting an infection of any kind.
Body Ecology uses fermented foods and beverages, food combining, and other principles to help establish and maintain a healthy environment inside your body that fights illness and disease.
In short: The Body Ecology program is ideal for helping to prevent bacterial, fungal, and viral infections and can be your top defense against sinusitis.
Whether or not you have sinusitis, the Body Ecology program offers a way to help build immunity, sustain energy, and prevent sickness and disease. You’ll have a much better chance of escaping cold and flu season — and circulating viruses — without the usual bouts of illness weakening your defense.
REFERENCES:
- 1. Mindy L. Seybold, DNP, ARNP, FNP-C. “Antobiotic stewardship and sinusitis: A quality improvement project,” The Journal of Urgent Care Medicine. 2020.
- 2. Ponikau JU, Sherris DA, Kern EB, Homburger HA, Frigas E, Gaffey TA, Roberts GD. The diagnosis and incidence of allergic fungal sinusitis. Mayo Clin Proc. 1999 Sep;74(9):877-84. doi: 10.4065/74.9.877. PMID: 10488788.
- 3. Braun H, Buzina W, Freudenschuss K, Beham A, Stammberger H. ‘Eosinophilic fungal rhinosinusitis’: a common disorder in Europe? Laryngoscope. 2003 Feb;113(2):264-9. doi: 10.1097/00005537-200302000-00013. PMID: 12567080.
- 4. Shetty, S., Chandrashekar, S. & Aggarwal, N. A Study on the Prevalence and Clinical Features of Fungal Sinusitis in Chronic Rhinosinusitis. Indian J Otolaryngol Head Neck Surg 72, 117–122 (2020). https://doi.org/10.1007/s12070-019-01769-w.
- 5. Nam, S.H., Chung, YS., Choi, Y.J. et al. Treatment outcomes in acute invasive fungal rhinosinusitis extending to the extrasinonasal area. Sci Rep 10, 3688 (2020). https://doi.org/10.1038/s41598-020-60719-7.
- 6. “Antibiotic Resistance Threats in the United States, 2019.” Centers for Disease Control and Prevention.