Your on-the-go gut care guide: Read this to avoid traveler’s diarrhea
Summer’s here, and many of us are itching to travel. After a year in relative isolation, though, is your microbiome ready for all that a vacation can throw at it? Nobody wants to miss seeing the sights, but traveling means different food, usually an altered sleep schedule, and maybe stress.
 Traveler’s diarrhea, caused often by E.coli, might well force changes to your itinerary. Looking after your microbiome while traveling, and before you go, can help everything go a little bit smoother.
Traveler’s diarrhea, caused often by E.coli, might well force changes to your itinerary. Looking after your microbiome while traveling, and before you go, can help everything go a little bit smoother.
Traveler’s diarrhea: What are your odds of getting it?
Millions of people experience traveler’s diarrhea every year. One meta-analysis found that the condition affects five to 50 percent of people, depending on travel destination, while in some high-risk areas, 50 to 90 percent of people may develop traveler’s diarrhea.1
In 2004, the United Nations World Tourism Organization found that a whopping 20 to 50 percent of the 170 million international travelers visiting countries in developing and tropical areas, such as Latin America, the Caribbean, the Middle East, South and Southeast Asia, and Africa, got sick with traveler’s diarrhea.2
And the biggest culprits? Contaminated food and water and sudden changes in diet.
Many things contribute to dysbiosis, though. These can include:
- Antibiotic therapy
- Environmental toxins
- Excess dietary sugar
- Food- and water-borne pathogens
- Hormonal changes
- Prolonged and severe stress
When traveling, location is a significant risk factor for developing so-called Delhi Belly, as are standards of accommodation, type of travel, and length of stay. How old you are can also affect your likelihood of getting sick, with older adults and very young children and infants most at risk.
So, what is traveler’s diarrhea?
- Most cases of diarrhea when traveling are the result of infection with enterotoxigenic Escherichia coli (ETEC) bacteria, although other pathogens are also to blame, such as Clostridium difficile and Campylobacter jejuni.
- These microorganisms attach themselves to the lining of the intestines, where they release toxins that draw water into the bowel, causing diarrhea and abdominal cramps.
- When it happens, traveler’s diarrhea tends to occur in the first week of travel, and symptoms can range from mild and brief to prolonged, severe, and painful.
In addition to diarrhea, travelers may experience other symptoms of dysbiosis, such as fatigue, immune system reactions, and even constipation.
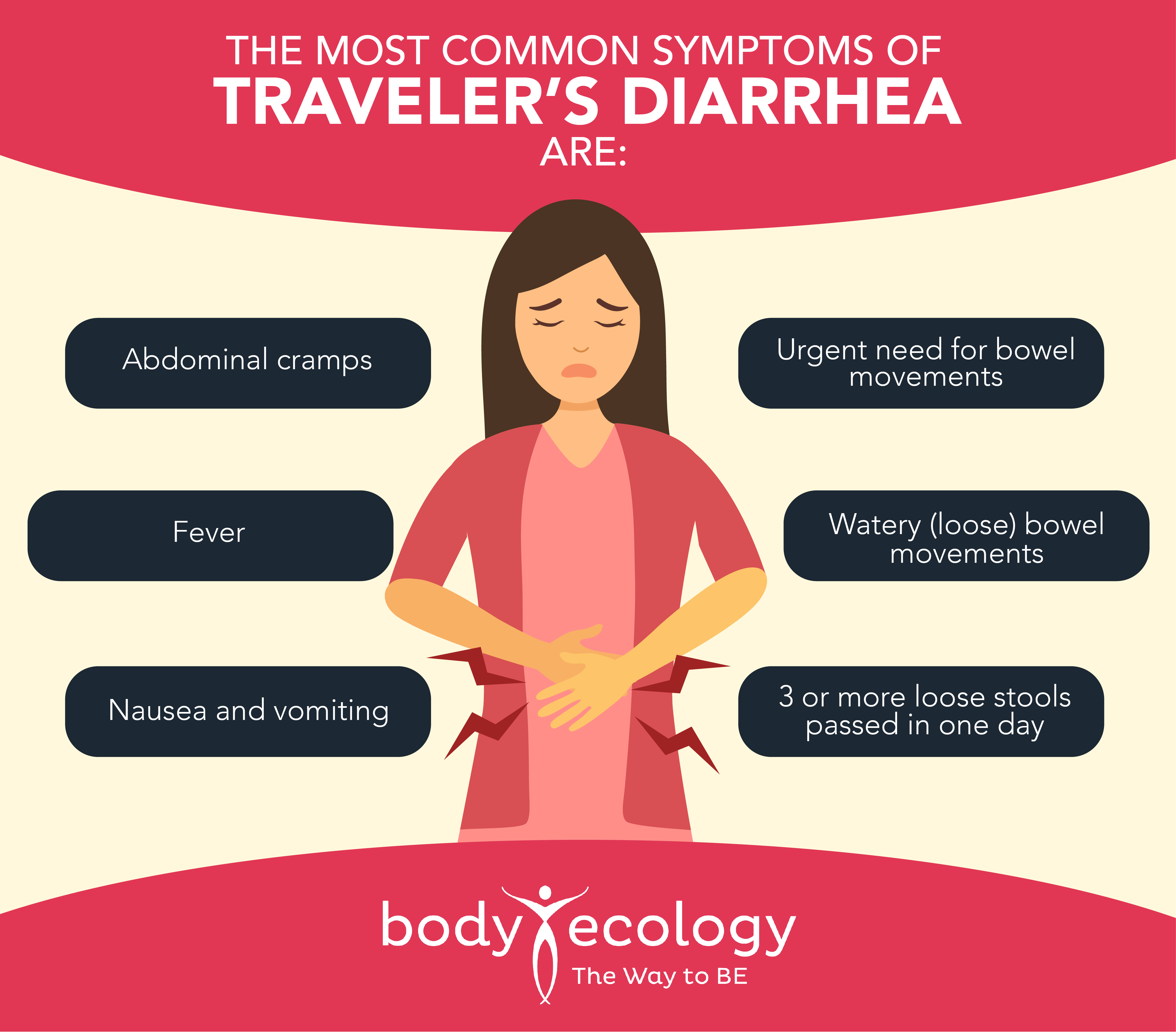
If diarrhea continues, signs of dehydration may arise, with fever, bloody stools, and severe abdominal or rectal pain being a sign it’s time to consult a physician. Some cases may require hospitalization and intravenous fluids to address serious dehydration that can otherwise prove fatal. In other cases, travel plans may need adjusting, and you might require bed rest.
For most people, though, traveler’s diarrhea can be resolved in a few days with immediate self-care. Better yet, taking proactive measures can help prevent traveler’s diarrhea in the first place.
Like deals? You’re going to love this.
No one wants traveler’s diarrhea: How to prevent it
Having a robust and diverse microbiome is, hands down, the best way to reduce your risk of traveler’s diarrhea.
This means taking steps to build and maintain your microbiome before traveling, and bringing shelf-stable travel probiotics with you on your trip. Supplementing digestive enzymes with hydrochloric acid (HCl) with each meal is wise since HCl digests protein in the stomach. (E. coli and other pathogens are a protein.)
In fact, your stomach is supposed to make this important stomach acid to protect you from pathogens entering your digestive tract when you eat. If you tend to find it hard to digest protein, and your stomach feels bloated for a few hours after a meal, this is a sign that you’re already lacking HCl anyway. (Blood type As tend to naturally be low in stomach acid, and stomach acid declines as we age.)
Saccharomyces boulardii, a beneficial yeast, has a range of benefits that can help prevent traveler’s diarrhea. These include:
- Helping suppress less desirable transient bacteria.3
- Lowering E. coli (EPEC) levels by 50 percent.4
- Producing beneficial short-chain fatty acids that support gut health.
- Protecting the gut from toxins produced by Clostridium difficile, another key culprit for diarrhea.5
- Reducing the pro-inflammatory response to E. coli and Candida albicans.6
A systematic review concluded that S. boulardii is effective in preventive and therapeutic treatment of 1) traveler’s diarrhea, 2) Clostridium difficile-associated diarrhea, and 3) acute diarrhea due to common viral and bacterial infections in children and adults.7
One placebo-controlled, double-blind study, involving 3,000 Austrian travelers, found that 250 mg and 1,000 mg of S. boulardii taken in advance of and continued while traveling significantly reduced the incidence of traveler’s diarrhea, with the higher dose more effective.8
Another study found that adult travelers (aged 19 to 69) with diarrhea who were given 150 to 450 mg of S. boulardii had much quicker recoveries.9
These travelers had suffered, on average, for 11 days prior to receiving the probiotic. After taking the supplements, most people recovered in five days. We have 10 billion S. boulardii per serving in our new GI Distress Relief™ (coming soon!), along with 40 billion Bifidus lactis (two standout strains) with research showing their benefit for gut dysbiosis.10
S. boulardii isn’t the only species that helps against traveler’s diarrhea:
- Lactobacilli and Bifidobacteria, for instance, produce lactic acid, which kills many food-borne pathogens that can cause traveler’s diarrhea.11
- Specifically, Bifidobacterium longum subsp. longum has been found to inhibit food-borne pathogenic bacteria.12
- Several studies also suggest that Lactobacillus helveticus R0052 can help prevent E. coli from sticking to human intestinal epithelial cells.13
- Likewise, L. helveticus R0052 seems to prevent E. coli from interfering with the function of cells lining the intestines.14
In another study, L. helveticus R0052 reduced Campylobacter jejuni invasion of human colon epithelial cells by 35 to 41 percent.15 C. jejuni is the most common bacterial cause of enterocolitis in humans.
Combating pathogens isn’t the only way that some probiotics help against traveler’s diarrhea. Through their effects on gut nerve cells, some probiotics, such as L. helveticus R0052 and B. longum R0175, may also help relieve symptoms, such as abdominal pain and feelings of anxiousness, that can accompany gastrointestinal upset when traveling.16
In general, probiotics are considered safe and effective for maintaining a healthy microbiome that’s better able to fend off undesirable bacteria, including E. coli. One meta-analysis of 34 randomized, blinded, controlled trials found that probiotics reduced the risk of traveler’s diarrhea by up to 21 percent and the risk of acute diarrhea of diverse causes by 34 percent (8 to 53 percent).17
Want to stay safe? Try these gut-friendly tips for travel
If you have a trip coming up, especially to an area where the water and food are at risk of pathogenic contamination, consider giving your gut some extra support:
- This might mean taking a probiotic supplement prior to travel, especially if you’ve had a recent course of antibiotics or recent gastrointestinal upset, or if you tend to suffer from dysbiosis.
- Include probiotic-rich foods in your diet for several weeks before traveling. Your baseline microbiome is likely to affect your susceptibility to traveler’s diarrhea, with greater gut diversity helpful in keeping symptoms at bay while away. Before you leave, focus on eating more fermented foods, like cultured veggies, sauerkraut, kimchi, and kefir.
- Definitely bring a bacteriophage product. EcoPhage is one product that should always come along on a trip; take it a few days before traveling and continue during and after a vacation ends. EcoPhage is a beneficial virus — a bacteriophage that’s only job is to kill E. coli. There are 10 phages for each bacteria in the world. You couldn’t ask for a better swat team standing guard day and night.
Travel-safe probiotics are those that contain shelf-stable strains that don’t require refrigeration to survive. If your accommodation and travel schedule allow, you might be able to put regular probiotics in your checked luggage with a cool pack as this stays cold during flights. Just remember to transfer the probiotics to the refrigerator in your hotel room or other accommodation once you arrive.
There’s a huge diversity of microbes in any one of Body Ecology’s three probiotic liquids. We can’t say this enough — “diversity is key!” Unparalleled diversity is found in cultured vegetables and our liquid probiotics.
In addition to probiotics, it’s a good idea to support your digestive health in other ways while traveling. Because you might be eating unfamiliar foods, and be less sure of the content of meals, digestive enzyme supplements can also be helpful. This is especially true if you know you have issues digesting gluten or lactose.
And finally, if you suspect that the food and water available to you while traveling may be contaminated, a biofilm-busting supplement can come in handy to kill stubborn pathogens. This is also useful to have on hand for when you get home, in case you brought back more than just some charming souvenir fridge magnets.
Caring for your microbiome before, during, and after a trip can make all the difference when it comes to dodging or minimizing traveler’s diarrhea. Here’s to a healthier vacation and happy travels.
REFERENCES:
- 1. McFarland, L.V. (2007). Meta-analysis of probiotics for the prevention of traveler’s diarrhea. Travel Med Infect Dis, Mar;5(2):97-105.
- 2. Diemert D. J. (2006). Prevention and self-treatment of traveler’s diarrhea. Clinical microbiology reviews, 19(3), 583–594. https://doi.org/10.1128/CMR.00052-05.
- 3. Moré, M.I., & Swidsinski, A. (2015). Saccharomyces boulardii CNCM I-745 supports regeneration of the intestinal microbiota after diarrheic dysbiosis – a review. Clin Exp Gastroenterol, Aug 14;8:237-55.
- 4. Czerucka, D., Dahan, S., Mograbi, B., Rossi, B., Rampal, P. (2000). Saccharomyces boulardii preserves the barrier function and modulates the signal transduction pathway induced in enteropathogenic Escherichia coli-infected T84 cells. Infect Immun, Oct;68(10):5998-6004.
- 5. Castagliuolo, I., Riegler, M.F., Valenick, L., LaMont, J.T., Pothoulakis, C. (1999). Saccharomyces boulardii protease inhibits the effects of Clostridium difficile toxins A and B in human colonic mucosa. Infect Immun, Jan;67(1):302-7.
- 6. Fidan, I., Kalkanci, A., Yesilyurt, E., Yalcin, B., Erdal, B., Kustimur, S., Imir, T. (2009). Effects of Saccharomyces boulardii on cytokine secretion from intraepithelial lymphocytes infected by Escherichia coli and Candida albicans. Mycoses, Jan;52(1):29-34.
- 7. Stier, H., & Bischoff, S.C. (2016). Influence of Saccharomyces boulardii CNCM I-745on the gut-associated immune system. Clin Exp Gastroenterol, Sep 13;9:269-279.
- 8. Kollaritsch, H., Holst, H., Grobara, P., Wiedermann, G. (1993). Prevention of traveler’s diarrhea with Saccharomyces boulardii. Results of a placebo controlled double-blind study. Fortschr Med, Mar 30;111(9):152-6.
- 9. Kirchhelle, A., Frühwein, N., Tobüren, D. (1996). Treatment of persistent diarrhea with S. boulardii in returning travelers. Results of a prospective study. Fortschr Med, Apr 20;114(11):136-40.
- 10. Engelbrektson A, Korzenik JR, Pittler A, Sanders ME, Klaenhammer TR, Leyer G, Kitts CL. Probiotics to minimize the disruption of faecal microbiota in healthy subjects undergoing antibiotic therapy. J Med Microbiol. 2009 May;58(Pt 5):663-670. doi: 10.1099/jmm.0.47615-0. PMID: 19369530.
- 11. Uraipan, S., & Hongpattarakere, T. (2015). Antagonistic Characteristics Against Food-borne Pathogenic Bacteria of Lactic Acid Bacteria and Bifidobacteria Isolated from Feces of Healthy Thai Infants. Jundishapur J Microbiol, Jun 1;8(6):e18264.
- 12. Johnson-Henry, K.C., Hagen, K.E., Gordonpour, M., Tompkins, T.A., Sherman, P.M. (2007). Surface-layer protein extracts from Lactobacillus helveticus inhibit enterohaemorrhagic Escherichia coli O157:H7 adhesion to epithelial cells. Cell Microbiol, Feb;9(2):356-67.
- 13. Jandu, N., Zeng, Z.J., Johnson-Henry, K.C., Sherman, P.M. (2009). Probiotics prevent enterohaemorrhagic Escherichia coli O157:H7-mediated inhibition of interferon-gamma-induced tyrosine phosphorylation of STAT-1. Microbiology, Feb;155(Pt 2):531-40.
- 14. Wine, E., Gareau, M.G., Johnson-Henry, K., Sherman, P.M. (2009). Strain-specific probiotic (Lactobacillus helveticus) inhibition of Campylobacter jejuni invasion of human intestinal epithelial cells. FEMS Microbiol Lett, Nov;300(1):146-52.
- 15. Diop, L., Guillou, S., & Durand, H. (2008). Probiotic food supplement reduces stress-induced gastrointestinal symptoms in volunteers: a double-blind, placebo-controlled, randomized trial. Nutrition Research, 28(1), l-5.
- 16. Sazawal, S., Hiremath, G., Dhingra, U., Malik, P., Deb, S., Black, R.E. (2006). Efficacy of probiotics in prevention of acute diarrhoea: a meta-analysis of masked, randomised, placebo-controlled trials. Lancet Infect Dis, Jun;6(6):374-82.
- 17. Stamps, Blake W et al. “A Pilot Study of the Effect of Deployment on the Gut Microbiome and Traveler’s Diarrhea Susceptibility.” Frontiers in cellular and infection microbiology vol. 10 589297. 15 Dec. 2020, doi:10.3389/fcimb.2020.589297.










