The Truth About UTIs

“My doctor told me it was Mr. Bubble,” my friend said.
“Seriously?” It didn’t make sense to me that a bubble bath could cause a bladder infection. But apparently, her doctor said that was how it started. My friend had had urinary tract infections (UTIs) since she was a little girl. She wasn’t having sex at 10 years old, so that wasn’t the problem, and the problem persisted into her twenties and thirties, and beyond. She didn’t really know what caused it, and for the most part, doctors had few answers.
For thousands of women, recurring bladder infections are something they are simply prone to getting. If left untreated, UTIs can develop into a kidney infection, which can be dangerous, even requiring hospitalization. Whether treated by a Gynecologist or by a Urologist, the treatment is usually the same: broad-spectrum antibiotics…until the infection clears (and the next one comes around.) This cycle would prove to wreak havoc on my friend’s microbiome.
Pathogens in the Urine
Medical science generally agrees that persistent pathogens (those difficult to eradicate), can remain in the body, contributing to chronic inflammatory conditions. Viral pathogens like those related to the herpes family of viruses can be at the root of chronic inflammation. Bacterial pathogens can also be problematic. Both can persist in the human body and contribute to different chronic inflammatory conditions.
Pathogens also exist in the gut microbiome but tend not to drive symptoms because they’re kept in check by the microbiome’s beneficial bacteria and a healthy immune system. But how they behave can change, making them more dangerous when the immune system is suppressed, or there is an imbalance of beneficial bacteria relative to pathogenic bacteria. Science is finding a growing number of persistent pathogens that can contribute to recurrent inflammatory conditions.
A Microbiome of its Own
Researchers have discovered that the gut is not the only organ with a microbiome. The bladder has a microbiome of its own. A 2021 study published in Frontiers in Cellular and Infection Microbiology using advanced computer sequencing, challenged the prevailing science that the bladder is a sterile organ. Scientists now believe that the bladder has its own microbiome, known as the urobiome. Under certain circumstances, changes to that microbiome can result in dysfunction, including UTIs.
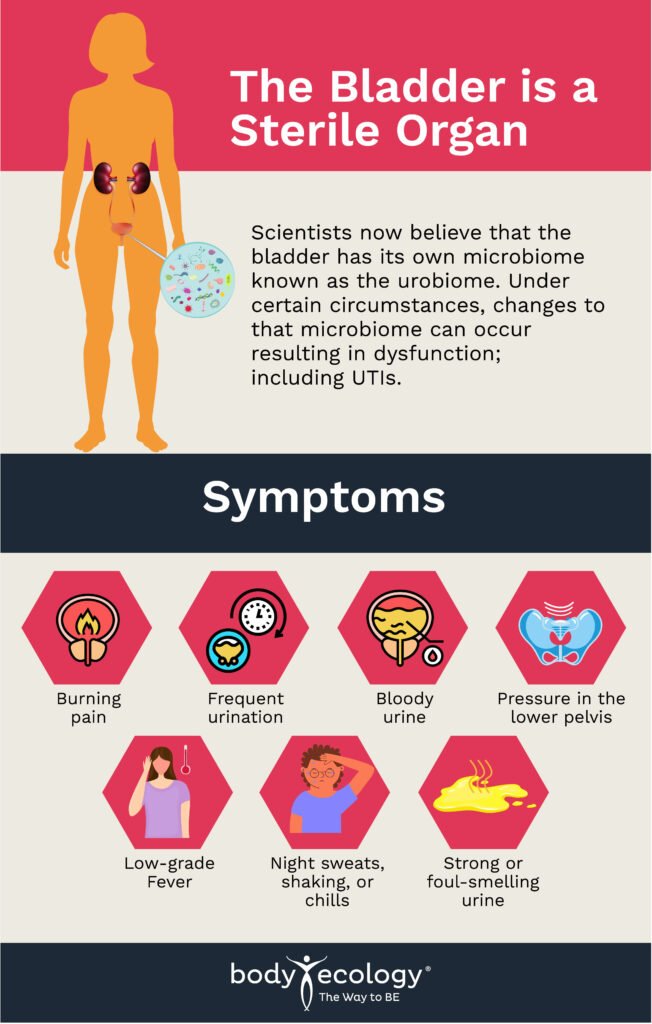
In 2018, a study examining female bladder bacteria was published in Nature. This study clearly showed that pathogenic bacteria could linger in the bladder (which, until very recently, was considered a sterile organ holding sterile urine). Some subjects in the study displayed no symptoms or were otherwise considered to have healthy bladder function, making study results even more striking.
A detailed comparison was made between the sampled bladder microbiota, the gastrointestinal microbiota and the natural vaginal microbiota. Not surprisingly, the vaginal and bladder microbiota were similar and functioned differently from what researchers observed in the gastrointestinal microbiota. Researchers identified some strains they considered to be pathogenic and also identified commensal, or neutral, bacteria typically found in healthy bladders.
In the study, 149 bacterial strains were isolated and analyzed from the samples taken. The urine collected included 78 species of bacteria representing a portion of the diversity of bacteria contained in those samples. Doctors noted in earlier studies that normal female urine shows quite a lot of diversity, including persistent bacteria previously shown to be associated with female bladder-related dysfunction.
In summary, the urogenital microbiota (the bacteria of the female bladder and the vagina), has its own unique, diverse, species of bacteria with healthy bacterial strains co-existing with pathogenic strains. So, what triggers the urinary tract infection?
The Old Standard of Care
When someone is seen by a doctor for a bladder infection, the doctor will usually order a urinalysis. The patient will often be prescribed an antibiotic based only on their symptoms, regardless of the bacterial strain causing the infection. E. Coli is typically the bacterial strain suspected to be causing the infection and is often the only strain tested. If the infection is deemed complicated, other bacterial species may be cultured.
This has been the standard of care for UTIs for the past sixty years (lab testing for high levels of E. Coli, and not much else.) Researchers are now beginning to look for other bacteria, fungi, and viruses in the bladder microbiomes of patients with UTIs. And they are finding these other organisms. Advances in computer modeling have given scientists a new window into just how persistent microbes in the bladder can be.
Bacteria, Viruses, and Fungi
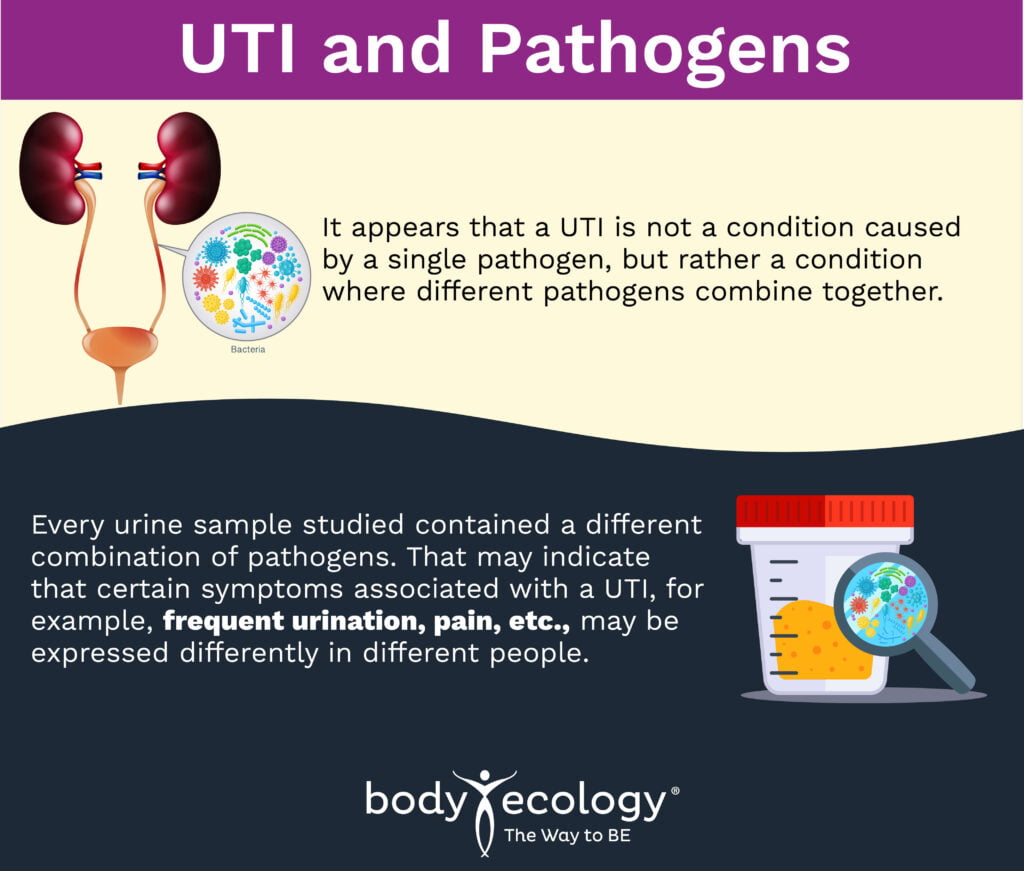
A UTI appears not to be caused by a single pathogen, but rather a condition where different pathogens combine. Every urine sample studied contained a different combination of pathogens. That may indicate that certain symptoms associated with a UTI, for example, frequent urination, pain, etc., may be expressed differently in different people.
On average, forty-one pathogenic species were found in samples taken from those with UTIs in the Nature study, confirming that pathogens are capable of enduring in UTIs. Furthermore, multiple fungal species were discovered, including several different candida species and various species of viruses. Every sample tested also had a range of bacterial, fungal and viral species.
Bacteriophages
There is another organism that may play a role in this cycle. A different 2018 study examined bacteriophages in the urine (viruses that infect bacteria and change the way the bacteria behave.) Researchers examined urine samples looking for bacteriophages. They looked at 181 bacteria that were persistent in the urine and found 457 associated bacteriophages capable of infecting those bacterial species in the urine samples. In this study, 226 of those bacteriophage species identified were predicted, (using advanced computer analysis), “with a high level of confidence.”
86% of the bacteria examined in the study contained at least one bacteriophage sequence with the ability of these viruses to infect bacteria. This adds to the new understanding of recurrent UTIs, making it necessary to include bacteriophages when considering what organisms might contribute to a UTI.
 One way to support beneficial microbes is with EcoPhage from Body Ecology. It selectively targets specific, harmful bacteria while leaving beneficial microbes to flourish. Supplementing with EcoPhage may help remove harmful, pathogenic bacteria and support gut health, helping to strengthen the overall immune system.
One way to support beneficial microbes is with EcoPhage from Body Ecology. It selectively targets specific, harmful bacteria while leaving beneficial microbes to flourish. Supplementing with EcoPhage may help remove harmful, pathogenic bacteria and support gut health, helping to strengthen the overall immune system.
New, sophisticated tools now enable scientists to gather much more comprehensive information. Identifying new organisms that can contribute to a UTI, to a different bladder condition, or simply that persist even in a healthy bladder, is an important advancement.
Interstitial Cystitis
A related bladder condition known as interstitial cystitis is a painful condition in which patients develop chronic bladder-related symptoms, such as lots of pain with urination, cramping, pain with sexual intercourse, and other symptoms. It is said to have no known cause.
With these patients, one will give a urine sample that will be sent to a “regular” laboratory, but the sample will not likely result in the finding of any microbes in that sample. That is because urine is believed to be sterile in patients with this condition.
Some studies have found that the urinary microbiome of people with interstitial cystitis is less diverse and is also associated with higher levels of pro-inflammatory cytokines (positive indicators of inflammation) than that of healthy subjects. More research is needed, but it is encouraging to see that interstitial cystitis will likely, going forward, be studied in an entirely different way.
Supporting a Healthy Bladder
How can someone support a healthy bladder? There are quite a few natural approaches to supporting healthy bladder function (starting with drinking LOTS of purified water to keep flushing out bacteria.) However, seeking medical attention for a bladder infection is important, particularly if blood is seen in the urine.
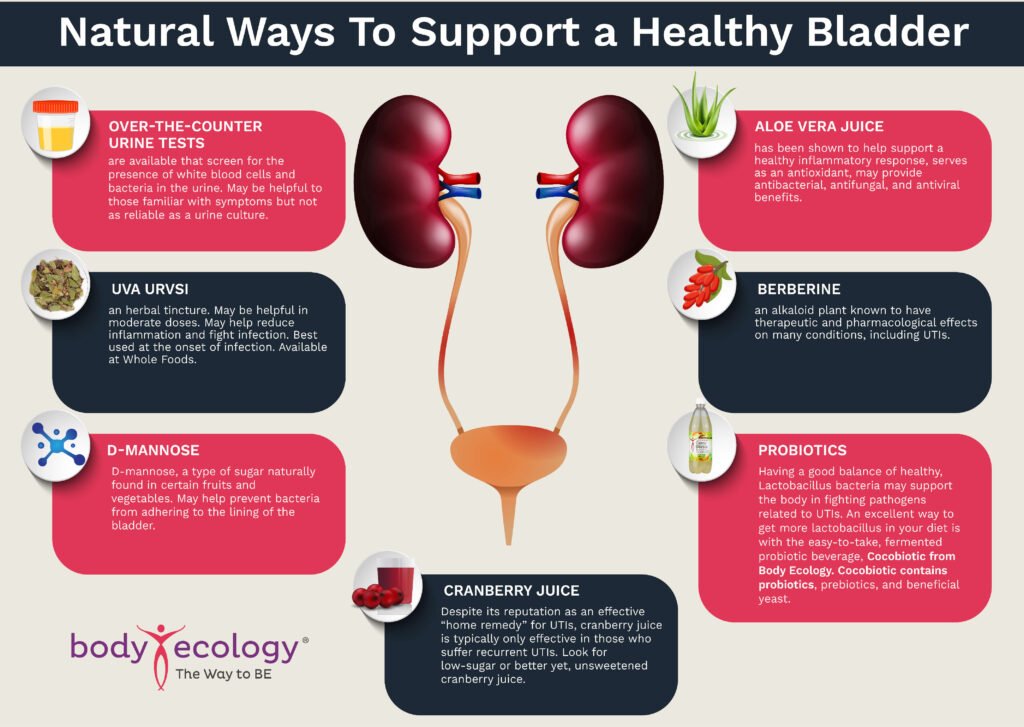
 Over-the-counter urine tests are available that screen for the presence of white blood cells and bacteria in the urine. These may be helpful to those familiar with symptoms but not as reliable as a urine culture from your doctor.
Over-the-counter urine tests are available that screen for the presence of white blood cells and bacteria in the urine. These may be helpful to those familiar with symptoms but not as reliable as a urine culture from your doctor.- Uva Ursi -an herbal tincture. May be helpful in moderate doses. May help reduce inflammation and fight infection. Best used at the onset of infection. Available at Whole Foods.
- D-mannose – D-mannose, a type of sugar naturally found in certain fruits and vegetables. May help prevent bacteria from adhering to the lining of the bladder.
- Aloe vera juice –has been shown to help support a healthy inflammatory response, is an antioxidant, and may provide antibacterial, antifungal, and antiviral benefits.
- Berberine – an alkaloid plant known to have therapeutic and pharmacological effects on many conditions, including UTIs.
- Probiotics – Having a good balance of healthy Lactobacillus bacteria may support the body in fighting pathogens related to UTIs. An excellent way to get more lactobacillus in your diet is with the easy-to-take, fermented probiotic beverages, Cocobiotic from Body Ecology. Cocobiotic contains probiotics, prebiotics, and beneficial yeast. A serving or more of fermented vegetables is a great prophylactic.
- EcoPhage from Body Ecology selectively targets specific, harmful bacteria while leaving beneficial microbes to flourish. Supplementing with EcoPhage may help remove harmful, E. coli pathogenic bacteria—a common culprit in UTIs. It can also serve as a prophylactic to prevent reoccurrence.
- Cranberry juice – Despite its reputation as an effective “home remedy” for UTIs, it is typically only effective in those who suffer recurrent UTIs. Look for unsweetened cranberry juice concentrate.