Long hauler? Autoimmune condition? Low DHEA impairs your recovery
In our series on COVID-19 and long haulers, we’ve already explored how a high level of the stress hormone cortisol has been associated with worse outcomes from SARS-CoV2 infection.

This time, we’ll look at another hormone — dehydroepiandrosterone (DHEA) — and its links to COVID-19 and long-lasting symptoms.
What is DHEA, and what does it do?
DHEA is a hormone made primarily by the adrenal glands and gonads (testicles and ovaries) but is also made in the brain and skin.
It’s the most essential and abundant steroid hormone, and under the right conditions, the body converts DHEA into sex hormones, such as testosterone and estrogen, helping to keep everything in balance.
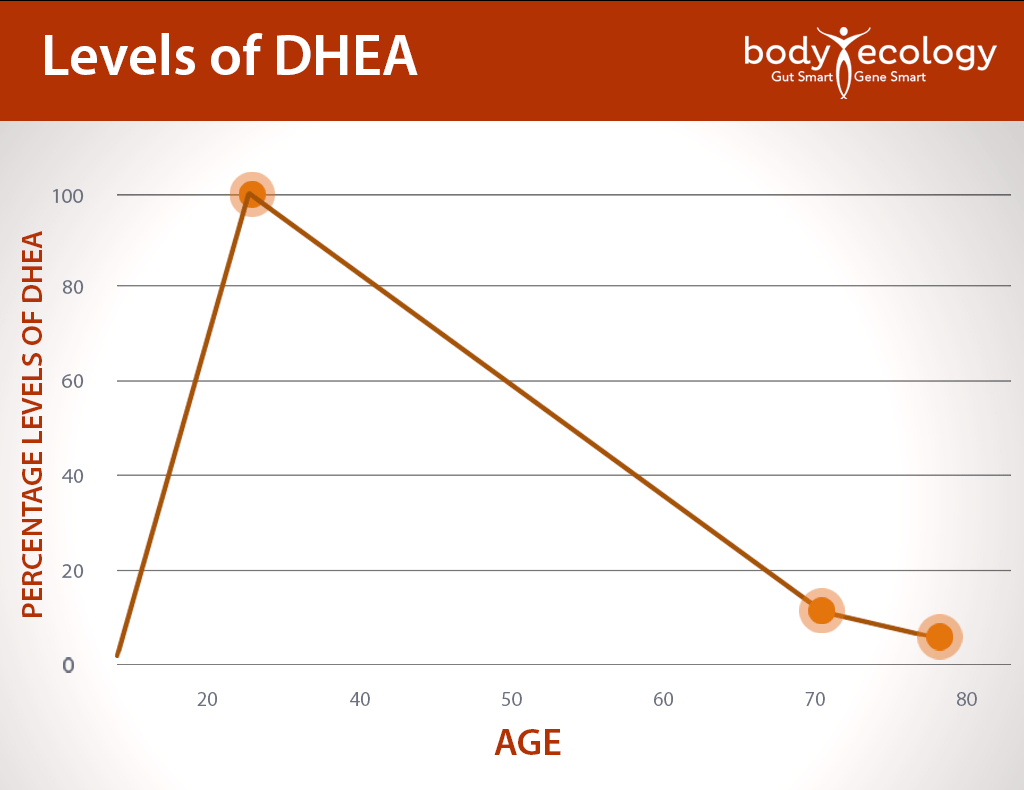
Usually, levels of DHEA decrease with age, peaking in early adulthood (around age 25) and then declining to about 10 to 20 percent of those levels by the age of 70 or 80.1
On top of that:
- DHEA decreases when we get sick or experience trauma.
- And, DHEA decreases with chronic, prolonged stress.
DHEA can help reduce chronically elevated cortisol levels, but only if you have enough in your body. Given that low levels of DHEA are associated with autoimmune diseases, many age-related diseases, and premature signs of aging, this is a critical hormone to monitor throughout your life. (Yes, starting even in your teens.)
If you’re tested and learn you have low levels of DHEA in your body — and are a long hauler or are trying to recover from an autoimmune condition — it’s important to address this. (Examples of common autoimmune conditions include Hashimoto’s, lupus, MS, psoriasis, rheumatoid arthritis, etc.)
*Note from the author: In my opinion, long haulers have the newest autoimmune condition.
DHEA may impact your body in several key ways:
1. Immune function.
DHEA is vital for immune function and helps to keep cortisol in check. DHEA and cortisol are antagonistic to each other. As mentioned, DHEA can help decrease chronic levels of cortisol — if you aren’t already running low. Like we saw earlier in this series, chronically elevated cortisol in cases of COVID-19 has been associated with an increased risk of death from the infection.
And so:
- A disruption in the balance of DHEA and cortisol may have a very negative effect on the immune system’s response to stress over the longer term.2
- For instance, DHEA has been shown to enhance the activity of Natural Killer cells and T lymphocytes, both of which help fight viral infections.3
DHEA has also been seen to reduce disease activity in autoimmune conditions, such as systemic lupus erythematosus, and to reduce the dose requirements for glucocorticoid medications (like prednisone or an equivalent).4
Do you know how to eat for optimal immune function? Download our free eBook now.
2. Other functions.
DHEA is also an effective anti-inflammatory agent, which gives it a role in helping to stave off age-related inflammatory diseases. One small crossover study examining the role of DHEA in aging men and women (40 to 70) noted that DHEA serum levels were restored to those found in young adults within two weeks of DHEA replacement and were sustained throughout the study.5
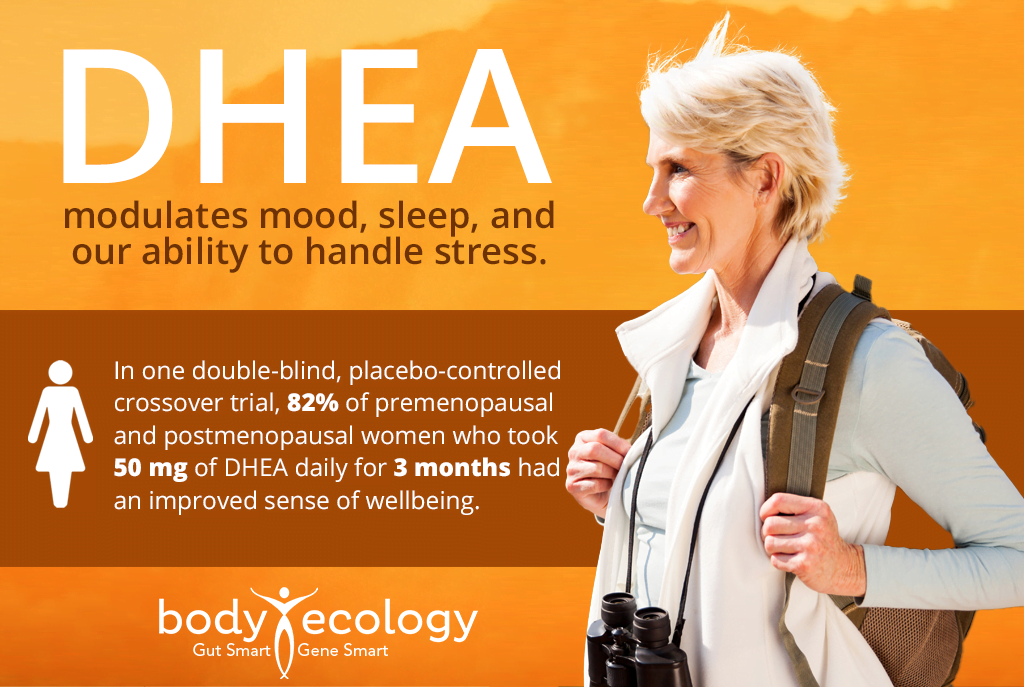
This meant better sleep quality, greater relaxation, increased energy, and more stress resilience (something we all need right now).
Could DHEA mitigate most negative effects of COVID-19?
Putting this all together, it’s not hard to see that DHEA may have an exceptionally important role to play in managing recovery from COVID-19.
COVID-19 has been shown to permanently damage the heart and blood vessels.6 DHEA is critical for cardiovascular health, with effects on nitric oxide levels, vascular tone, cholesterol, and blood pressure.7
COVID-19 may also trigger unresolved, ongoing inflammation and might adversely impact cognitive and emotional wellbeing.
Exhaustion and weakness are a common complaint of those with an infection, of long haulers, and of anyone with an autoimmune disease. If you suffer from Hashimoto’s — an autoimmune condition affecting the thyroid gland — DHEA is needed to turn the thyroid hormone T4 into T3, the form needed by every cell in the body for energy. Cortisol prevents T4 from converting to T3. And again, DHEA can reduce cortisol if you have enough.
Some clinicians have suggested that the replacement of DHEA will help combat the so-called “adrenal fatigue.”8 It takes energy to heal, so finding ways to increase energy is essential.
One study looked at levels of DHEA (and its breakdown product or “metabolite” DHEA-sulfate) after an infection or injury. They found that cortisol continued to increase — and DHEAS decreased — and finally peaked at two weeks. DHEAS levels did not return to normal even six months later.9 The suggestion to replace DHEA levels to restore energy just makes good sense.
Taking DHEA as a supplement is not for everyone though and could have dangerous side effects, especially if you’re already taking medications, are pregnant, or have pre-existing medical conditions.
For anyone with an autoimmune disorder or long hauler symptoms, you really need to find a healthcare provider who can test you and is knowledgeable about cortisol, DHEA, adrenal fatigue, and conditions like POTS. The DUTCH hormone test is our preferred method of testing. You can locate a practitioner trained in administering and interpreting the test by going to their website. You can also consult with a doctor via telemedicine.
Thankfully, there are ways to help increase your DHEA levels without using a supplement. Focus on rest and getting more sleep. This’ll help support your energy levels and adrenals, which produce DHEA. On that note, minimize stress wherever possible — which may help to deepen your sleep while simultaneously helping to lower insulin and cortisol, both of which are at odds with DHEA.
Upping your intake of healthy fats is also a smart move. Your body needs omega-3 fatty acids to manufacture cholesterol, which is a primary building block of DHEA. So, enjoy more ghee, olive oil, coconut oil, flaxseed oil, and raw butter with your meals, and read more here for extra tips to help naturally balance DHEA.
Also, taking 7-keto-DHEA as a supplement can be a safer way to raise your DHEA levels without continuing down the pathway to make testosterone and estrogen, like taking DHEA does. Women naturally produce about 8 to 10 mg of DHEA per day. But if you’re deficient, you’ll need to take more. So again, testing is important with this hormone.
COVID-19 is proving itself to be an incipient disease, with a dizzying range of symptoms that may defy diagnosis without proper, holistic attention. By reducing stress and cortisol levels and taking steps to raise DHEA, long haulers may see some relief from persistent symptoms. This is valuable information for anyone with an autoimmune condition as well.
REFERENCES:
- 1. Samaras N, Samaras D, Frangos E, Forster A, Philippe J. A review of age-related dehydroepiandrosterone decline and its association with well-known geriatric syndromes: is treatment beneficial?. Rejuvenation Res. 2013;16(4):285-294. doi:10.1089/rej.2013.1425.
- 2. Vermes I, Beishuizen A. The hypothalamic-pituitary-adrenal response to critical illness. Best Pract Res Clin Endocrinol Metab. 2001 Dec;15(4):495-511. doi: 10.1053/beem.2001.0166. PMID: 11800520.
- 3. Sebastiano Bruno Solerte, Marisa Fioravanti, Giulio Vignati, Andrea Giustina, Luca Cravello, Ettore Ferrari, Dehydroepiandrosterone Sulfate Enhances Natural Killer Cell Cytotoxicity in Humans Via Locally Generated Immunoreactive Insulin-Like Growth Factor I, The Journal of Clinical Endocrinology & Metabolism, Volume 84, Issue 9, 1 September 1999, Pages 3260–3267, https://doi.org/10.1210/jcem.84.9.6003.
- 4. Petri MA, Lahita RG, Van Vollenhoven RF, Merrill JT, Schiff M, Ginzler EM, Strand V, Kunz A, Gorelick KJ, Schwartz KE; GL601 Study Group. Effects of prasterone on corticosteroid requirements of women with systemic lupus erythematosus: a double-blind, randomized, placebo-controlled trial. Arthritis Rheum. 2002 Jul;46(7):1820-9. doi: 10.1002/art.10364. PMID: 12124866.
- 5. Morales AJ, Nolan JJ, Nelson JC, Yen SS. Effects of replacement dose of dehydroepiandrosterone in men and women of advancing age. J Clin Endocrinol Metab. 1994 Jun;78(6):1360-7. doi: 10.1210/jcem.78.6.7515387. Erratum in: J Clin Endocrinol Metab 1995 Sep;80(9):2799. PMID: 7515387.
- 6. Tushar Kotecha, Daniel S Knight, Yousuf Razvi, Kartik Kumar, Kavitha Vimalesvaran, George Thornton, Rishi Patel, Liza Chacko, James T Brown, Clare Coyle, Donald Leith, Abhishek Shetye, Ben Ariff, Robert Bell, Gabriella Captur, Meg Coleman, James Goldring, Deepa Gopalan, Melissa Heightman, Toby Hillman, Luke Howard, Michael Jacobs, Paramjit S Jeetley, Prapa Kanagaratnam, Onn Min Kon, Lucy E Lamb, Charlotte H Manisty, Palmira Mathurdas, Jamil Mayet, Rupert Negus, Niket Patel, Iain Pierce, Georgina Russell, Anthony Wolff, Hui Xue, Peter Kellman, James C Moon, Thomas A Treibel, Graham D Cole, Marianna Fontana, Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance, European Heart Journal, 2021;, ehab075, https://doi.org/10.1093/eurheartj/ehab075.
- 7. Arlt W, Hammer F, Sanning P, Butcher SK, Lord JM, Allolio B, Annane D, Stewart PM. Dissociation of serum dehydroepiandrosterone and dehydroepiandrosterone sulfate in septic shock. J Clin Endocrinol Metab. 2006 Jul;91(7):2548-54. doi: 10.1210/jc.2005-2258. Epub 2006 Apr 11. PMID: 16608898.
- 8. Beishuizen A, Thijs LG, Vermes I. Decreased levels of dehydroepiandrosterone sulphate in severe critical illness: a sign of exhausted adrenal reserve? Crit Care. 2002 Oct;6(5):434-8. doi: 10.1186/cc1530. Epub 2002 Jul 9. PMID: 12398784; PMCID: PMC130144.
- 9. Mark A Foster, Angela E Taylor, Neil E Hill, Conor Bentley, Jon Bishop, Lorna C Gilligan, Fozia Shaheen, Julian F Bion, Joanne L Fallowfield, David R Woods, Irina Bancos, Mark M Midwinter, Janet M Lord, Wiebke Arlt, Mapping the Steroid Response to Major Trauma From Injury to Recovery: A Prospective Cohort Study, The Journal of Clinical Endocrinology & Metabolism, Volume 105, Issue 3, March 2020, Pages 925–937, https://doi.org/10.1210/clinem/dgz302.